Internal and Disaster Medicine Integration (Part 2 of 3)
Nicole Gunawansa | May 27th, 2015
This interview was held on April 15th, 2015 in Tohoku Medical Megabank Building
Part 2- Disaster Medicine Experience of a ToMMo Clinical Fellow
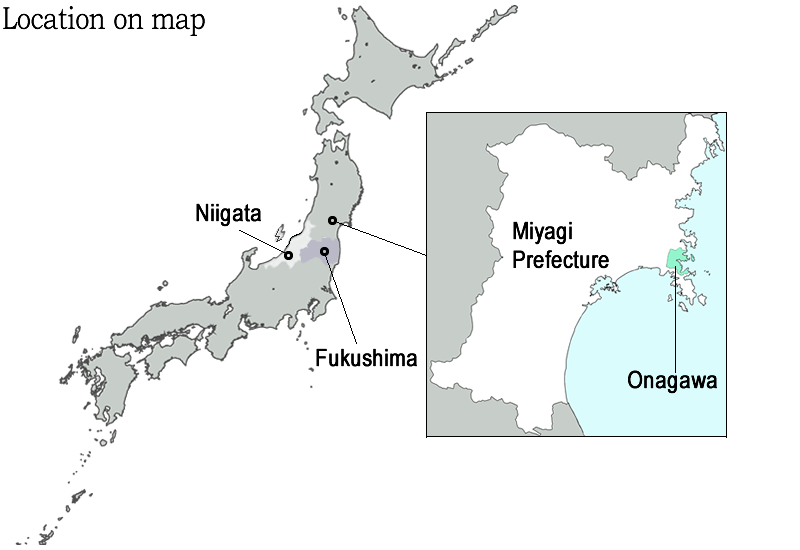
Question 4: Please describe what is like to work as a physician in Onagawa, a city greatly affected by the earthquake and tsunami four years ago?
The first two year after the disaster, I worked in Onagawa one or two times a month to see psychosomatic and internal medicine patients who deal with disorder either before or after 3/11. I noticed that the stress of the disaster impacted conditions such as diabetes and hypertension, most like because of a lack of nutritional and medical resources following the earthquake/tsunami. The exacerbation and promotion of these health conditions was integrally connected to disaster mental stress. For example, I saw a male 38 year old patient with back pains. After my evaluation, I discovered that his pain originated after/during his search for his wife’s body immediately after 3/11. These types of physical ailments, related to mental distress, were not just seen in adults. I also worked with some school children that did not/could not go to school because of the grief they felt that their friends had families, but they did not after the disaster.
While working in Onagawa, I learned that we could not manage these patients with only medicine because their problems were not just physical, but also involved mental distress. At Onagawa Community Medical Center, physicians take time to listen to the thoughts and feelings of their patients. No reservations are necessary, and patients are always welcomed and accommodated for depending on doctors’ availability because we want to help resolve both the physical and mental pain of the survivors.

Dr. Tanaka (center) and her colleagues in front of the Onagawa Community Medical Center (May, 2015)
Back in 2004 in Niigata, I felt satisfaction with my group’s volunteer efforts, and after two months we finished our project because people were successfully moving out of the evacuation centers. The 2011 disaster feels very different from the one in Niigata as there is no end to the disaster relief period, only a beginning.
I feel deeply connected to the Onagawa community, and feel a sense of obligation to promote disaster medicine research to help rebuild the community. Until recently, disaster medicine lacked internal medicine. For example, Disaster Medical Assistance Team (DMAT) primary focus is surgical and trauma related. This is not the case with internal medicine; we have to follow patients after the disaster and be concerned with their family systems, housing, employment situation, and social interaction as all of these factors affect internal physicians’ medical decisions/recommendations. The disaster radically changed how internal medicine was viewed in relation to disaster medicine, and so now there is an increased interest in the role of stress in diseases like Irritable Bowel Syndrome (IBS).
Question 5: As a gastroenterologist, do you feel there has been an increase in gastroenterological disorders following the disaster in 2011?

Dr. Tanaka appeared as a guest on the Onagawa Saigai FM Radio's talk show (June 27th, 2014)
I don’t have an actual figure, but my impression is that the number of gastroenterological (GI) disorders in patients has been increasing. Normally endoscopies are performed once a week in Onagawa, and these patients have often expressed new onset of stomach or internal problems after the disaster. Essentially, eating impacts the function of GI syndrome and psychological problems, which intern influences hormones and the gut. Since lifestyles have been changed after 3/11, I am hoping to do more research evaluating this area.
As a member of the ToMMo Clinical Fellow Program (TCF), my group tries to solve community medicine problems and help decrease the work load of overworked physicians by distributing specialty physicians appropriately. In Onagawa, 1000 patients receive endoscopies in one year so that these patients do not have to visit Ishinomaki Red Cross Hospital. Strategic placement of doctors helps to reduce the burden not only in that town, but in other areas as well. For instance, I can say with confidence that a trained doctor can help educate young nurses and hospital staff, thus increasing sustainability in medical care in those affected areas. Collaboration amongst medical professions at different facilities can help promote sustainability, and incentives to building such relationships include the ability to express different shared experiences/abilities at these local hospitals.
Question 6: Having been exposed to survivors suffering with stressful mental health conditions, what have you learn about disaster psychiatry and disaster medicine post 3/11?
I noticed after the 2011 disaster, some patients suffer from not only mental health conditions but also physical such as hypertension. These are often psychologically induced internal symptoms. The anxiety that these patients feel often negatively impacts their mental health, which often results in sleep loss, decreased immune capabilities, and internal disorder development. A lot of the patients in internal medicine have issues that originate from mental distress. Most physicians in internal medicine and gastroenterology want concrete data, but psychiatrists sometimes cannot provide this data, and a discrepancy between these areas develops. The field of psychosomatics hopes to bridge this communication gap by providing evidence. ToMMo data (blood samples, psychiatric evaluations, etc.) can help partially solves this communication problems and promote more effective patient care.
 |
 Reconstruction of Onagawa bay area has a long way to go (June, 2014) |